
|
|
|||||
|
|
|
|
|
|
|
YOUR LATEST ISSUE ABOUT MRCP PACES IS HERE!
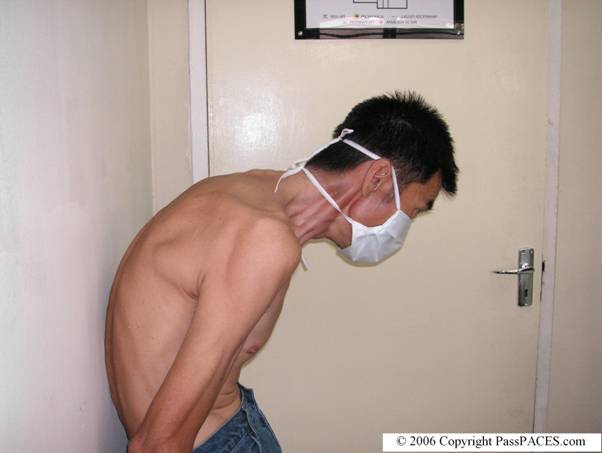
Inspect this gentleman and proceed.

Discussion:
OK, this is a common case in MRCP PACES station 5 if you are sitting the exam in Malaysia and Singapore. I think it is easy for you to detect the abnormality in this gentleman because the clinical signs are obvious. You notice this gentleman has severe spine abnormalities. Yes, you are right, he has ‘Question mark’ posture. This is due to fixed kyphoscoliosis of the thoracic spine with compensatory extension of the cervical spine. This case is easy but you must remember to look for these spine abnormalities especially if you are seeing a patient who is lying in bed during your MRCP PACES exam because the kyphoscoliosis may not be obvious and can be masked by a pillow behind the patient’s back.
Patients with Ankylosing Spondylitis usually present with back pain and this gentleman has chronic back pain since the age of 20 years old. Proceed to do the following after a general inspection,
![]() ask the patient to walk away from you and turn back and walk towards you. Pay attention to patient’s posture.
ask the patient to walk away from you and turn back and walk towards you. Pay attention to patient’s posture.
![]() ask patient to look to either side. You will notice patient may have limited cervical spine movement. The patient may need to move his whole body when he wants to look to either side.
ask patient to look to either side. You will notice patient may have limited cervical spine movement. The patient may need to move his whole body when he wants to look to either side.
![]() check his thoracic and lumbar spine movement , usually, I would ask patient to flex aside(lateral flexion), rotate and do forward and backward flexion. Remember to fix the patient pelvis when you ask patient to do rotation. You will notice patient with Ankylosing Spondylitis has very limited spine movement.
check his thoracic and lumbar spine movement , usually, I would ask patient to flex aside(lateral flexion), rotate and do forward and backward flexion. Remember to fix the patient pelvis when you ask patient to do rotation. You will notice patient with Ankylosing Spondylitis has very limited spine movement.
![]() you need to do two tests to demonstrate the patient has limited spine movement by demonstrating ‘occiput to wall’ test and Schober’s test. In following picture, when I ask the patient to rest his back against the wall, you notice that this gentleman has difficulty to make contact his head against the wall.
you need to do two tests to demonstrate the patient has limited spine movement by demonstrating ‘occiput to wall’ test and Schober’s test. In following picture, when I ask the patient to rest his back against the wall, you notice that this gentleman has difficulty to make contact his head against the wall.
![]() for Schober’s test, mark two points, one 10 cm above and one 5 cm below a line joining the ‘dimple of Venus’ on the sacral promontory. An increase in the separation of less than 5 cm when the patient does a forward flexion signifies limited spine movement.
for Schober’s test, mark two points, one 10 cm above and one 5 cm below a line joining the ‘dimple of Venus’ on the sacral promontory. An increase in the separation of less than 5 cm when the patient does a forward flexion signifies limited spine movement.
![]() after these tests, check peripheral joints especially hands and also look for possibility of psoriasis ( because one variant of psoriatic arthropathy may look like Ankylosing spondylitis)
after these tests, check peripheral joints especially hands and also look for possibility of psoriasis ( because one variant of psoriatic arthropathy may look like Ankylosing spondylitis)
![]() suggest to examiners you will like to look for 4As- Anterior uveitis, Apical fibrosis, Aortic regurgitation and Achilles tendinitis.
suggest to examiners you will like to look for 4As- Anterior uveitis, Apical fibrosis, Aortic regurgitation and Achilles tendinitis.
Common questions examiners would ask you,
1)
What are the diagnostic criteria to diagnose Ankylosing Spondylitis?
2)
How do you manage this gentleman?( Remember that genetic counseling is important and remember to talk about HLA-B27!)
Conclusion:
This gentleman has Ankylosing Spondylitis with limited spine movement.
Extra points:
1) Diagnostic criteria of Ankylosing Spondylitis is based on New York Criteria (1966)
![]() Limitation of motion of the lumbar spine in all 3 planes: anterior flexion, lateral flexion and extension.
Limitation of motion of the lumbar spine in all 3 planes: anterior flexion, lateral flexion and extension.
![]() History of the presence of pain at the dorsolumbar junction or in the lumbar spine.
History of the presence of pain at the dorsolumbar junction or in the lumbar spine.
![]() Limitation of chest expansion to 1 inch (2.5 cm) or less, measured at the level of the fourth intercostal space
Limitation of chest expansion to 1 inch (2.5 cm) or less, measured at the level of the fourth intercostal space
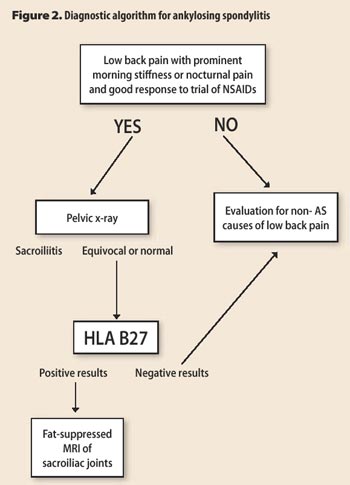
2) I find the following algorithm interesting and helpful,
| Case ID: 2 | Created: 29 September 2006 |
Station 2: You are the SHO in charge of Medical Clinic.
Subject: Mr Lee, 54-year old
Kindly see Mr Lee who has recently been complaining of chest pain for the past 2 months. He has previous history of Myocardial Infarct about 5 years ago and bypass was done 4 years ago. I am worried whether the pain is cardiac in origin. He has history of hypertension and diabetes mellitus for the past 10 years and currently under my follow up. I also notice his blood pressure is not controlled and his last fasting blood sugar and HbA1C were 9.0 and 7.2%.I would appreciate if you can help me to manage this patient.
You have 14 min until the patient leaves the room followed by 1min for reflection before the discussion with the examiners.
Discussion:
A popular question in MRCP PACES station 2. A patient presents with chest pain. Remember that besides cardiac pain , you must also consider other types of pain which may mimic chest pain, diagnoses to consider include ischaemic heart disease ( either stable, unstable angina or myocardial infarct), pulmonary embolism, pericarditis, reflux oesophagitis, musculoskeletal pain, penumonia ( pleuritic chest pain)... etc.
When you want to take further history of pain, always remember to take the following details,
![]() nature of the pain, whether it is similar to his previous pain before bypass surgery
nature of the pain, whether it is similar to his previous pain before bypass surgery
![]() duration of the pain (each episode)
duration of the pain (each episode)
![]() any radiation
any radiation
![]() precipitating and relieving factors
precipitating and relieving factors
![]() other associated symptoms
other associated symptoms
However, it is not enough you just get the diagnosis in this patient, you also notice besides diagnosis problem in this case, you are seeing management problems as well, Mr Lee's hypertension and diabetes mellitus are not properly managed. You must ask relevant questions so that his medical problems can be properly managed such as
![]() compliance to treatment
compliance to treatment
![]() other risk factors for ischaemic heart disease such as high cholesterol, smoking and family history
other risk factors for ischaemic heart disease such as high cholesterol, smoking and family history
![]() his normal diet and exercise
his normal diet and exercise
Never assume anything before entering the examination room, always bear in mind all the possible differential diagnoses and ask relevant questions to come to a provisional diagnosis.Also avoid spending all your time in getting your provisional diagnosis because there may be other important issues to deal such as social problems, impact of the disease towards patient's daily life, drug history.......etc
Summarize your history before you present to the examiners and outline your plan of management. Issue that concerns the patient and his GP most is whether the pain is cardiac in origin, you should be able to answer this question at the end of your interview!
Source:
1) 250 Cases in Clinical Medicine, RR Baliga
2) EVALUATION OF DIAGNOSTIC CRITERIA FOR ANKYLOSING SPONDYLITIS: A COMPARISON OF THE ROME, NEW YORK AND MODIFIED NEW YORK CRITERIA IN PATIENTS WITH A POSITIVE CLINICAL HISTORY SCREENING TEST FOR ANKYLOSING SPONDYLITIS
HENK SIMON GOEI THE, MALCOLM M. STEVEN, SJEF M. VAN DER LINDEN and ARNOLD CATS , British Society of Rheumatology, 1985
3) The College of Family Physicians of Canada
To see previous issues, click here! To send a quick comment, click here!